Sometimes you don't have an insurance card or payer information - just a patient's name, date of birth, and address. The Discovery API fills that gap, helping your app identify active coverage before running any eligibility or benefit checks.
How Discovery Works
- Minimal inputs: Typically
firstName,lastName,dateOfBirth, andstate - Search and match: Discovery queries payer networks and other data sources to find potential coverage matches
- Optimised for speed: The first successful match is returned via webhook (P95 < 15 seconds) to ensure the patient is not kept waiting
- False positives:
zipCodecan be included in the request to filter out any false positives that might be returned
Webhooks
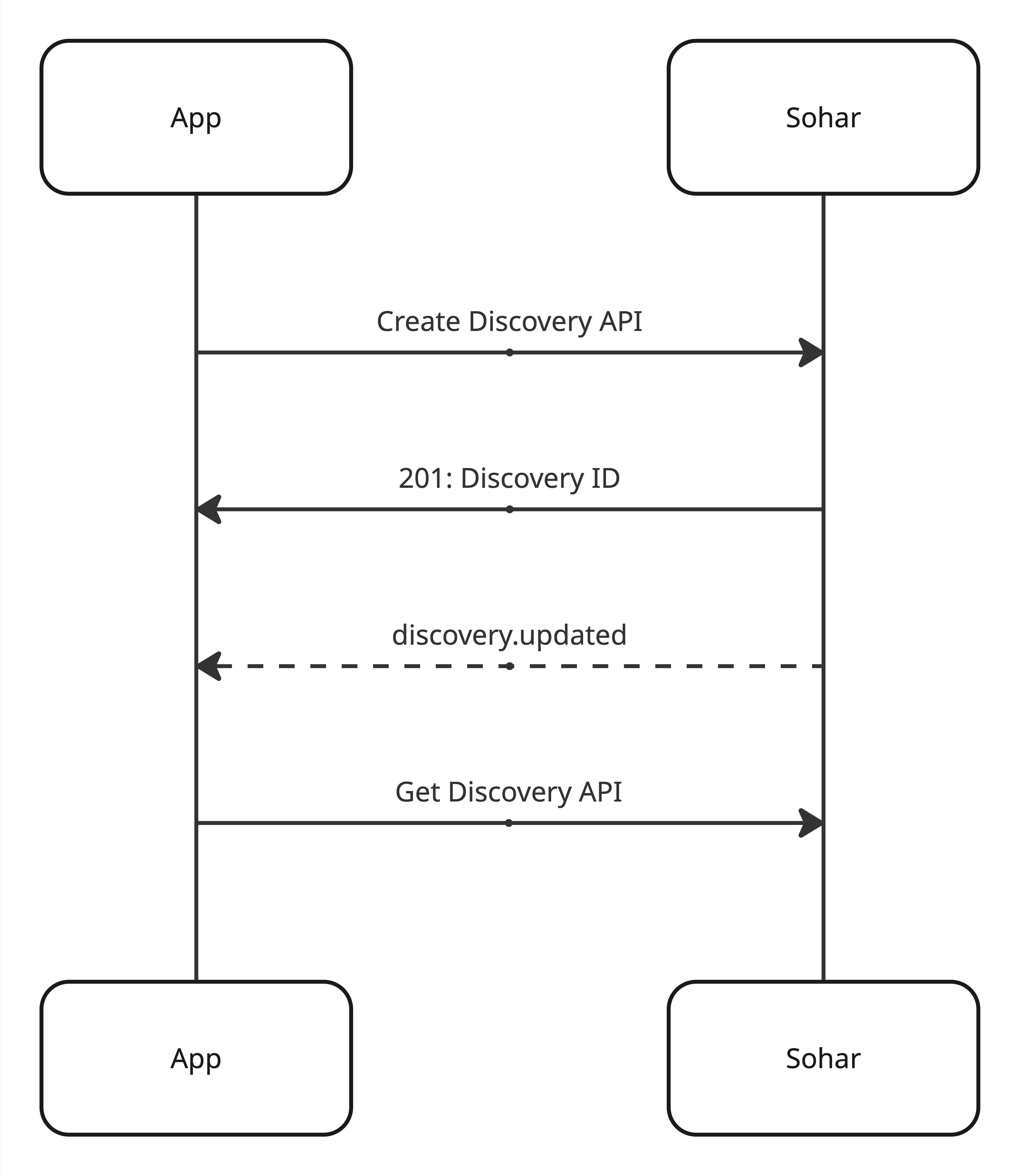
As with other asychronous Sohar APIs, webhooks are our recommended approach.
- Immediate updates when a match is found
- Minimal polling/infra noise
- Easy to build out API orchestrations
Polling
If you can't host webhooks yet, poll the Get Discovery API until the status is no longer "pending".
- Poll with backoff (e.g., 1s → 2s → 4s → stop by 1m or earlier if done)
- Stop polling when the status is not "pending"
We can build upon our polling function for Verification, making it generic to also handle the Discovery API.
async function waitForResponse<T extends { status: string }>(
url: string,
maxDurationMs: number // e.g. 24 * 60 * 60 * 1000 for 24h, or 60 * 1000 for 1m
): Promise<T> {
let delay = 1000;
const deadline = Date.now() + maxDurationMs;
while (Date.now() < deadline) {
const response = await api<T>(url);
if (response.status !== "pending") return response;
await new Promise((resolve) => setTimeout(resolve, delay));
delay = Math.min(delay * 2, 15000);
}
throw new Error("response_timeout");
}What You Get Back
If successful, a complete Discovery response includes:
- Payer information: the matched payer name and ID
- Member data: member ID and updated demographic information
Practical Guidance
- Clean inputs: Even minor typos or formatting errors can affect match quality
- Cache results: Reuse Discovery results across the patient's next visits or re-verifications
- Use Verification next: Discovery is designed as a precursor - once you know the payer, confirm coverage through Verification
Where This Fits in Flows
- Discovery → Verification: Find the payer, then confirm eligibility and benefits
- Discovery → Verification → Cost Estimate: Go from unknown coverage to full transparency
- Verification → Discovery: Identify a secondary payer for coordination of benefits
