Once you've identified a patient's payer, the next question is: "Are they covered?" Verification answers that asynchronously so your app stays fast and resilient.
How Verification Works
- Fire-and-forget: You submit a Verification request, we immediately return an ID
- Processing window: We resolve the request typically in seconds (P90 = 10 seconds) with a maximum resolution time of 24 hours for edge cases
- No client retries needed: While a request is processing, a call to the Get Verification API will return a "pending" status until it's complete
- One check per month: Eligibility rarely changes daily, cache results and re-verify monthly (or sooner if the patient reports a change)
Webhooks
Best for real-time UX and fewer network calls - this is our recommended approach.
- Immediate updates when payers respond
- Minimal polling/infra noise
- Easy to build out API orchestrations
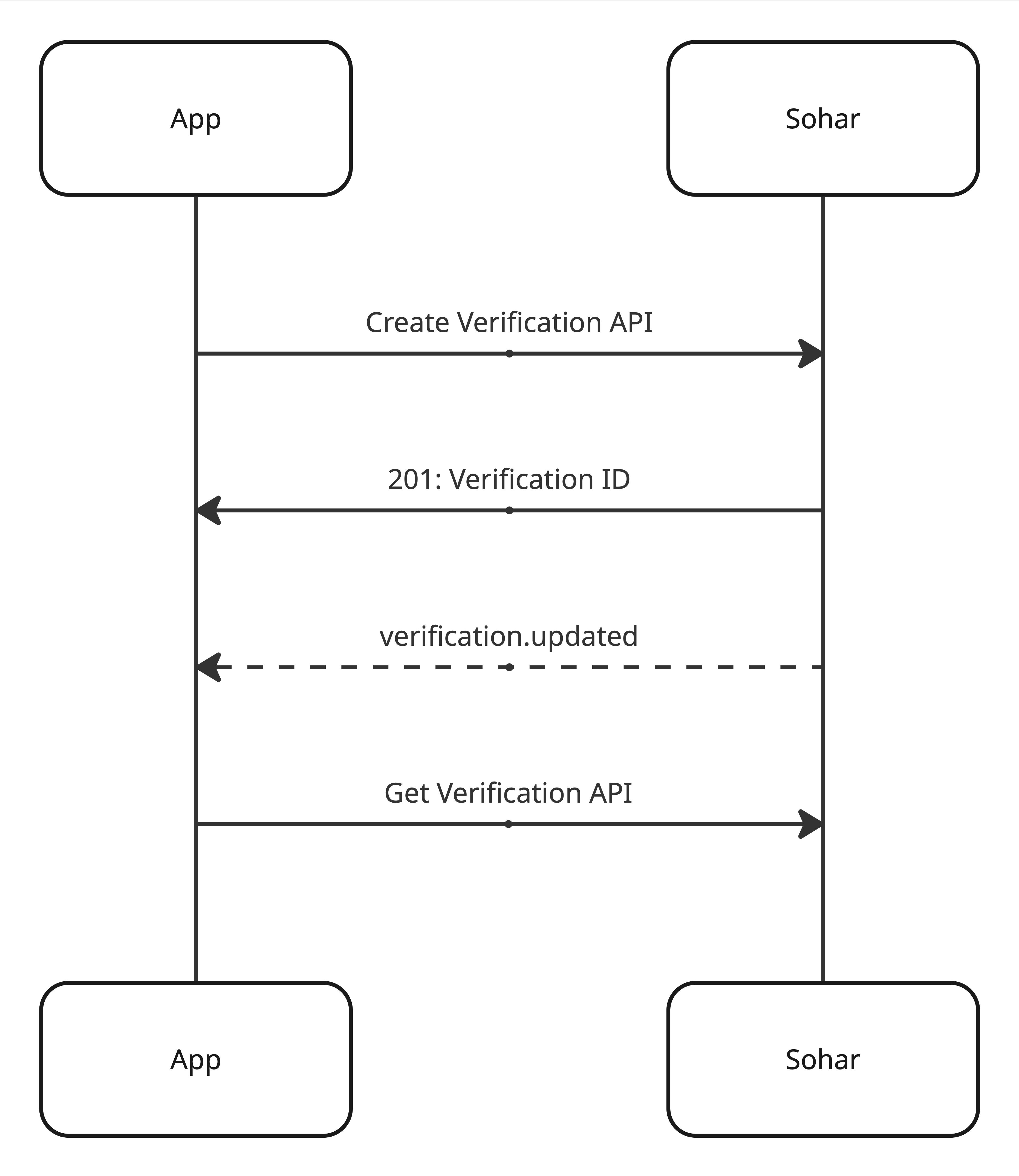
Polling
If you can't host webhooks yet, poll the Get Verification API until the status is no longer "pending".
- Poll with backoff (e.g., 1s → 2s → 4s → stop by 24h or earlier if done)
- Stop polling when the status is not "pending"
async function waitForVerification(id) {
let delay = 1000;
const deadline = Date.now() + 24*60*60*1000;
while (Date.now() < deadline) {
const v = await api(`/v2/verifications/${id}`);
if (v.status !== "pending") return v;
await new Promise(r => setTimeout(r, delay));
delay = Math.min(delay * 2, 15000);
}
throw new Error('verification_timeout_24h');
}What You Get Back
When complete, a Verification includes:
- Eligibility: eligible/ineligible and a timestamp
- Plan details: plan name, coverage dates
- Benefits: copay, coinsurance, deductible, out-of-pocket
Store and display the Verification payload and timestamp until the beginning of the next month.
Practical Guidance
- Don't retry POSTs for "time out" concerns - just use the returned
verificationIdand wait (webhook or GET) - Monthly cadence: Re-verify on a schedule (e.g., first of the month) or on patient-triggered events (new card, appointment scheduled)
- Downstream chaining: Once the request is complete, trigger Network Status automatically
Where This Fits in Flows
- Discovery → Verification: confirm coverage after finding the payer and member ID
- Verification → Network Status: determine network status for the patient