Healthcare coverage is complicated. Eligibility checks, benefits verification, network status, and cost estimates often happen in silos, leaving patients and providers frustrated. At Sohar, we believe these steps can be orchestrated into smooth, automated flows - just like modern software systems are stitched together through APIs.
That's what this new series - Flows - is about. Each week, we'll explore a practical way to combine our APIs into workflows that solve real-world problems. Think of it like a recipe book: sometimes we'll keep it simple, sometimes we'll chain together multiple ingredients to create something more powerful.
The Four Building Blocks
At the core of Flows are our four APIs:
- Verification - Confirm a patient's coverage and return detailed benefits information
- Discovery - Find coverage when you don't know the payer
- Network Status - Determine whether a patient's provider is in-network
- Cost Estimate - Return a breakdown of expected costs for a given patient and procedure
You can use each API on its own, but the real magic comes from orchestration: chaining them together into workflows that mirror real-life healthcare processes.
Example: A Simple Flow
Let's start small. Imagine a clinic has a new patient who arrives without their insurance card. How do you handle it?
Here's a basic Flow:
- Discovery - Using just demographic info (name, date of birth, state), you identify the payer
- Verification - Once the payer is found, you immediately verify eligibility and retrieve benefits
In practice, this looks like:
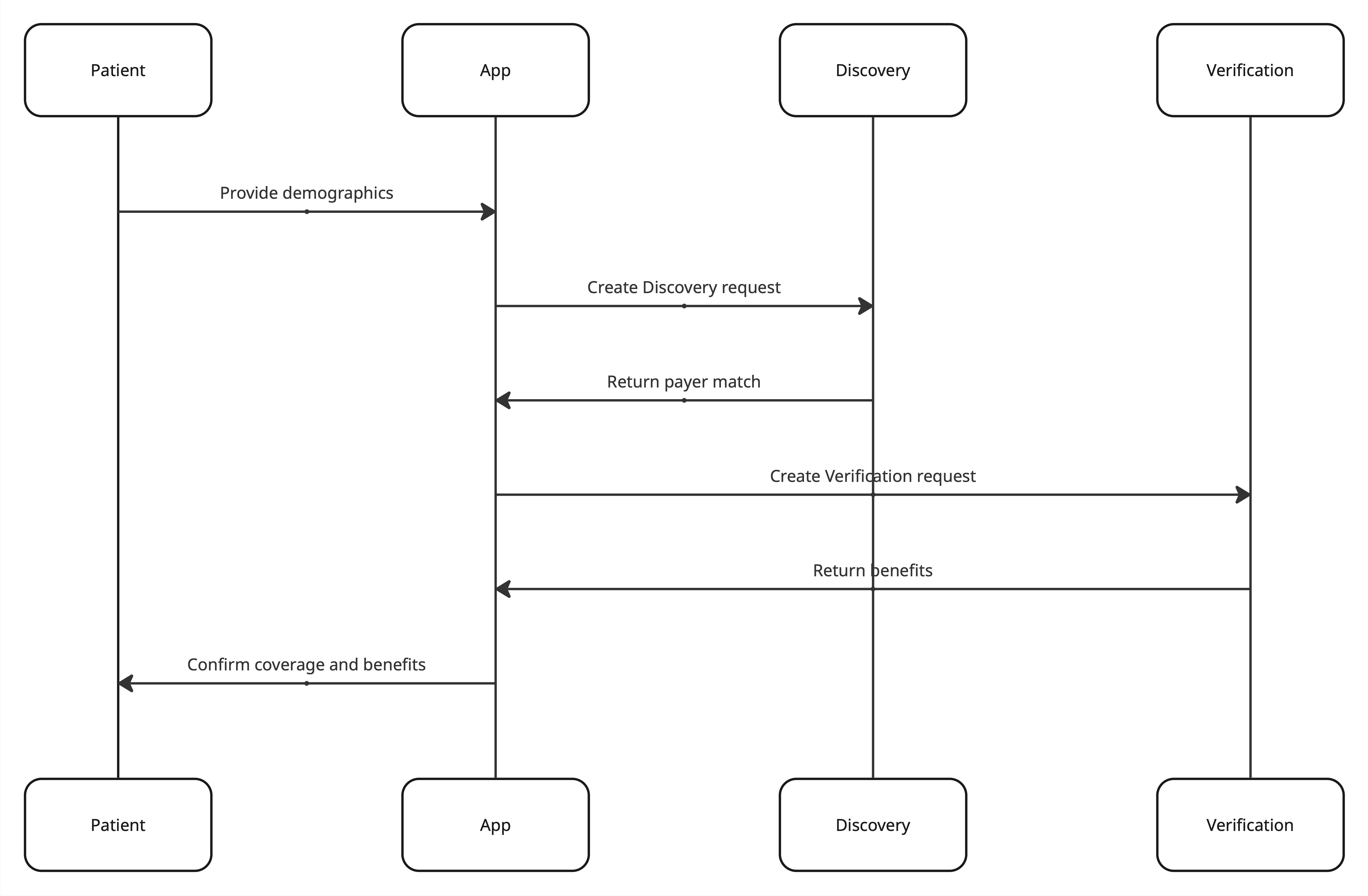
This flow ensures the front desk doesn't need to chase insurance details, and the patient can move forward with confidence.
Why Flows Matter
- For developers: Flows reduce complexity. Instead of building custom integrations for every clearinghouse, you orchestrate standardized APIs
- For providers: Flows speed up intake, reduce denied claims, and improve scheduling accuracy
- For patients: Flows provide clarity - no more guessing about coverage or costs
What's Next
Each week we'll walk through Flows ranging from the simple (like this Discovery → Verification recipe) to the complex (like coordinating benefits across multiple payers or providing real-time surgical cost estimates).